1 aug 2018
Turns out that the kind of heart attack that I had (caused by a 95% blockage in the big left anterior descending coronary artery) – the so-called widowmaker heart attack – may actually be relatively uncommon in women. You might guess that fact by its nickname. It’s not, after all, called the “widower-maker”.
While cardiologists warn that heart disease can’t be divided into male and female forms, there are some surprising differences. Cardiologist Dr. Amir Lerman at the world famous Mayo Clinic in Rochester, Minnesota, told the Los Angeles Times recently:
“When it comes to acute heart attacks and sudden death from cardiac arrest, women have these kinds of events much more often without any obstructions in their coronary arteries.”
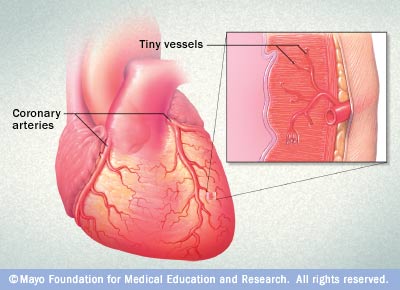
Instead, it appears that a significant portion of women suffer from another form of heart disease altogether. It affects not the superhighway coronary arteries but rather the smaller arteries, called microvessels. These tiny arteries deliver blood directly to the heart muscle.
Ironically, I can now boast two diagnoses for the price of one – first, the widowmaker heart attack caused by a fully occluded coronary artery back in 2008, and then, after several months of puzzling, ongoing cardiac symptoms – like chest pain, shortness of breath, and crushing fatigue – a second diagnosis of inoperable coronary microvascular disease.
In 2006, research published in the journal Circulation looked at the Women’s Ischemia Syndrome Evaluation (WISE) study data on almost 1,000 women referred for cardiac testing due to their symptoms(1). Here’s what they found:
- 62% had non-obstructive coronary artery disease – defined as blockages less than 50% of the artery
- 17% had one coronary artery vessel significantly blocked or narrowed
- 11% had two vessels narrowed
- fewer than 10% had three vessels affected
Dr. Noel Bairey Merz, a cardiologist at Cedars-Sinai Medical Center in Los Angeles, headed up the WISE study, which began in 1996. The average age of her participants was 58, but a quarter were younger and pre-menopausal.
Researchers found that what’s known as ischemic heart disease (any decreased blood flow and oxygen to the heart muscle) is often caused by a blockage within one or more coronary arteries that are feeding the heart muscle, but can also be due to at least two other possibilities:
- dysfunction of the smallest coronary microvascular arteries
- coronary spasm
1. CORONARY MICROVASCULAR DISEASE
They used a test in which doctors first measured blood flow through the heart and then injected a drug that should have made the arteries dilate and increased the flow. If the flow did not rise, the patient most likely had microvascular disease.
One third of the women in the L.A. study had low blood flow to the heart muscle caused by coronary microvascular disease. For these women, the rate of deaths or heart attacks was higher than would be expected for other women with normal angiograms.
According to the Texas Heart Institute, coronary microvascular disease most likely happens when small blood vessels in the heart tighten or constrict. This tightening reduces the blood flow to the heart muscle and causes the pain of angina pectoris (a Latin phrase that means “strangling in the chest“).
The encouraging news at first: because these vessels are so tiny, early research suggested that they may not increase the risk of a heart attack or death. But the Journal of the American Medical Association reported in 2005 that the prognosis of patients with unstable angina and non-obstructive coronary artery disease is not benign and includes a 2% risk of death or heart attack at 30 days of follow-up(2). (JAMA. 2005;293(4):477-484. doi: 10.1001/jama.293.4.477)
Problematically, coronary microvascular arteries are too small to detect with the standard cardiac tests that cardiologists would normally use to see larger vessels, so women in particular are often dismissed and sent home with a misdiagnosis in spite of severe and distressing cardiac symptoms.
For example, in typical patients with coronary artery disease, coronary angiography – considered the ‘gold standard’ of cardiac diagnostics – usually shows a clearly blocked artery that slows blood flow to the heart muscle.
But in patients with coronary microvascular disease, these test results are normal – even though symptoms may be as debilitating as those experienced during a heart attack.
Dr. Noel Bairey Merz adds that angiograms that would clearly spot blockages in major heart arteries can miss coronary microvascular disease altogether. As a result, many women who have gone to their doctors with chest pain have gone home with a clean bill of heath – and most likely feeling very embarrassed for having made a fuss over nothing. She says:
“Historically, women have been told that it was in their head.”
According to the Harvard Heart Letter, the preferred diagnostic tool for correctly identifying coronary microvascular disease is coronary reactivity testing.
“Coronary reactivity testing is an angiogram-like test lasting 60 to 90 minutes; it allows doctors to see how very small vessels supplying the heart respond to different ‘challenges’ from medications. “
Texas Heart Institute experts tell us that up until recently, the only treatment for coronary microvascular disease (also sometimes known as Cardiac Syndrome X, a name that’s generally hated by those of us diagnosed with MVD because of its implication that this disorder somehow doesn’t exist!) has been with these medications:
- Nitroglycerin (nitro) can widen or dilate the arteries and improve blood flow to your heart. Nitro can be given through a skin patch, pills, an ointment, or a spray.
- Beta blockers “block” the chemical or hormonal messages sent to your heart. When you are under physical or emotional stress, your body sends signals to your heart to work harder. Beta-blockers block the effect these signals have on your heart, so they reduce the demands on your heart.
- Calcium channel blockers can help to keep your arteries open and reduce your blood pressure by relaxing the smooth muscle that surrounds the arteries in your body. The oxygen demand of the heart is also reduced by these medicines.
Physical exercise has also been shown to be helpful in managing MVD symptoms. A Swedish study reported in the Journal of the American College of Cardiology in 2000 suggested that being out-of-shape is a “prominent feature” in patients diagnosed with MVD. Researchers found that a 30-minute workout on an exercise bike three times a week resulted in increased exercise capacity with lesser chest pain for the MVD patients they studied.
As more physicians become educated about the widespread incidence of coronary microvascular disease, particularly in women patients, more treatments are becoming available.
2. CORONARY SPASM DISORDERS
Another example of non-obstructive heart disease often seen in women is called Prinzmetal’s Variant Angina, chest pain caused by a spasm of a coronary artery. While Prinzmetal’s is not thought to cause a heart attack, chances of a cardiac event are higher in those with underlying heart conditions.
We don’t yet know exactly what causes coronary spasms like Prinzmetal’s.
One theory lies within the thin lining of the blood vessels called the endothelium. Usually this artery lining produces a chemical (nitric oxide) that helps to widen the blood vessel, allowing blood to flow through with ease.
But if the artery lining is damaged or isn’t working properly, the blood vessel may narrow and cause a coronary spasm. Levels of the artery-widening chemical are higher when estrogen levels are also high at certain stages of the menstrual cycle. A 2001 study published in the journal, Annals of Internal Medicine, suggested that during times when estrogen levels are high, women have fewer chest pain symptoms(3). In addition, smokers tend to have lower levels of nitric oxide in their blood vessels than non-smokers, and smoking is a major risk factor for coronary spasm.
Symptoms of angina can also occur in the absence of any coronary artery disease. Up to 30% of people with a heart valve problem called aortic stenosis, which can cause decreased blood flow to the coronary arteries from the heart, can have angina. People with severe anemia may have angina because their blood doesn’t carry enough oxygen. People with thickened heart muscles need more oxygen and can have angina when they don’t get enough.
We do know that cardiovascular disease kills more women than any other cause, about six times more women each year than breast cancer does, and in fact, more than all forms of cancer combined. Each year since 1984, more women than men have died of cardiovascular disease. Men tend to develop heart disease on average 10 years earlier than women do.
Anatomically, male and female hearts look about the same. When healthy, both should be about the size of a fist (a man’s heart is the size of a man’s fist, and a woman’s heart is smaller because it’s about the size of a woman’s fist). If you’re a woman, yours weighs about the same as a green pepper and, also like a green pepper, has hollow chambers inside.
Both men and women have three main coronary arteries surrounding their hearts. These are the large blood vessels that wrap around the outside of the heart, supplying blood, oxygen and nutrients to heart muscle to keep each heart pumping properly – and thus the arteries most susceptible to life-threatening cardiac events through obstructive – or non-obstructive – heart conditions.
But women who have a heart attack far worse right after the event and also suffer a poorer quality of life.

Geef een reactie